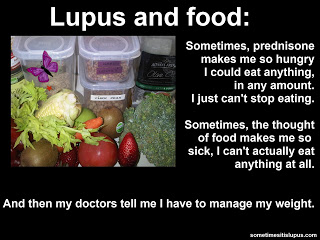
 Those of us taking steriods often struggle to lose weight (or even to stop gaining weight), let's revisit the basics of weight control with an expert in the field of food.
Those of us taking steriods often struggle to lose weight (or even to stop gaining weight), let's revisit the basics of weight control with an expert in the field of food.The following post, by Clare Collins, Professor in Nutrition and Dietetics, University of Newcastle has been republished from The Conversation. See the original version here: https://theconversation.com/health-check-six-tips-for-losing-weight-without-fad-diets-52496
Health Check: six tips for losing weight without fad diets
Clare Collins,
University of Newcastle
Monday - start diet. Tuesday - break diet! Wednesday - plan to start again next Monday.
If this is you, it’s probably time to get off the diet roller coaster and make some bigger changes to the way you eat, drink and think about food.
Here are six tips to help you get started.
1. Improve your diet quality score
When trying to lose weight, it might be tempting to quit carbs, dairy or another food group altogether.But to stay healthy, you need to meet your requirements for important nutrients like iron, zinc, calcium, vitamins B and C, folate and fibre. These nutrients are essential for metabolism, growth, repair and fighting disease.
Our review of diet quality indexes used to rate the healthiness of eating habits found that eating nutritious foods was associated with lower weight gain over time.
Improving your diet quality means eating more fruit and vegetables, lean meats, poultry, fish, eggs, tofu, nuts and seeds, legumes, dried beans, wholegrains and dairy (mostly reduced fat).
Rate your diet quality and get brief feedback using our online Healthy Eating Quiz www.healthyeatingquiz.com.au.
2. Mum was right - eat your veggies
Fruit and veg are high in fibre, vitamins and phytonutrients, but low in total kilojoules. So eating more can help you manage your weight.A study of more than 130,000 adults found that those who increased their intake of fruit and vegetables over four years lost weight. For each extra daily serve of vegetables, there was a weight loss of 110 grams over the four years. It was 240 grams for fruit. Small, but it all adds up.

Drilling down to specific fruit and veg gets interesting. Increasing cauliflower intake was associated with a four-year weight reduction of about 620 grams, with smaller reductions for capsicum (350g), green leafy vegetables (230g) and carrots (180g). The reduction was 620g for blueberries and 500g for apple or pears.
It was not good news all round, though. Corn was associated with a weight gain of 920g, peas 510g and mashed, baked or boiled potatoes 330g.
3. Limit your portion size
If you are served larger portions of food and drinks, you eat more and consume more kilojoules. That sounds obvious, yet everybody gets caught out when offered big portions - even when you’re determined to stop when you’re full.Research shows offering larger portions leads adults and children to consume an extra 600 to 950 kilojoules (150-230 calories). This is enough to account for a weight gain of more than seven kilograms a year, if the kilojoules aren’t compensated for by doing more exercise or eating less later.
4. Watch what you drink
A can of softdrink contains about 600 kilojoules (150 calories). It takes 30-45 minutes to walk those kilojoules off, depending on your size and speed.Children and adolescents who usually drink a lot sugary drinks are 55% more likely to be overweight.
Switch to lower sugar versions, water or diet drinks. A meta-analysis of intervention studies (ranging from ten weeks to eight months) found that adults who switched had a weight reduction of about 800 grams.
5. Cue food
Our world constantly cues us to eat and drink. Think food ads, vending machines and chocolate bars when trying to pay for petrol or groceries. Food cues trigger cravings, prompt eating, predict weight gain and are hard to resist. They can make you feel hungry even if you are not.
Try to minimise the time you spend in highly cued food environments. Avoid food courts, take a list when you go to the supermarket and take your own snacks to places where highly palatable food is advertised, like the movies.
This will reduce autopilot eating, which sabotages your willpower.
6. Resist temptation
A treatment for food cue reactivity is called exposure therapy. With the help of a psychologist or health professional, you expose yourself to the sight and smell of favourite foods in locations that commonly trigger overeating, like eating chocolate when watching TV. But, rather than eat the chocolate, you only have a taste without eating it.Over time, and with persistence, cravings for chocolate reduce, even when cues such as TV ads or people eating chocolate in front of you are present.
You can also draw on your brain’s own self-management skills to resist temptation, but it takes conscious practice. Try this food cue acronym, RROAR (remind, resist, organised alternative, remember and/or reward), to train your brain to resist temptation on autopilot.
When you feel yourself pulled by cues to eat or drink:
- Remind yourself that you are the boss of you, not a food cue.
- Resist the tempting food or drink initially by turning your back on the cue. (This gives you time to think about next steps.)
- Have a pre-Organised Alternative behaviour to use against food cues. Grab a drink of water, walk around the block, check your phone messages, read, take a walk in the opposite direction. Diversion works.
- Remember what your big-picture goal is. Do you want to eat better to help you feel better, reduce medications, lower blood pressure, improve diabetes control or manage your weight?

You need a plan
The journey off the diet roller coaster needs a cunning plan. Here’s how you can put it all together.- Start by assessing your diet quality using the Healthy Eating Quiz.
- Next, plan weekly meals, drinks and snacks. Write a grocery list and buy extra fruit and vegetables.
- Swap to small plates, cups and serving utensils. You’ll serve and eat less without thinking.
- Aim for half your plate covered with vegetables and salad, one-quarter lean protein (trimmed meat, chicken, fish, legumes) and one-quarter grains or starchy vegetables (potato, peas, corn).
- Change your food environment to avoid constant prompts to eat.
- Minimise the places you allow yourself to eat and drink to reduce food cue exposure (not in front of TV or computer, at a desk, or in the car).
- Keep food out of sight (unless it is fruit and vegetables). Store in opaque containers.
- Remove workplace food displays, such as food fundraisers.
- Plan driving and walking routes that do not take you past fast-food outlets or vending machines.
- Prerecord TV shows and fast-forward food ads.
Clare Collins, Professor in Nutrition and Dietetics, University of Newcastle
This article was originally published on The Conversation. Read the original article.